This leaflet is to help you understand what Pulmonary atresia is, what tests you need, and the implication of being diagnosed for you, your baby, and your family.
What is pulmonary atresia with intact ventricular septum (PA-IVS)?
Pulmonary atresia with intact ventricular septum encompasses a group of cardiac anomalies that have in common a complete obstruction of the valve that connects the right ventricle (RV) and the pulmonary artery that carries blood to the lungs, in the presence of an intact interventricular septum.
RV size will depend on the function of the tricuspid valve. Thus, two types of PA-IVS can be distinguished:
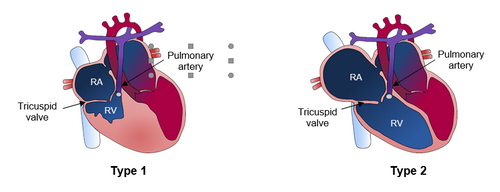
Type 1: The tricuspid valve is functioning well. Blood enters the right ventricle but there is an obstruction at the outlet of the right ventricle and the blood cannot move forward. As the tricuspid valve works well, blood cannot flow backward. There is a lot of pressure inside the right ventricle. The increased pressure makes it difficult for blood to flow into the right ventricle. With too little blood passing through the ventricle, the right ventricle does not develop.
Type 2: The tricuspid valve is not functioning properly. Blood enters the right ventricle but there is an obstruction at the outlet of the right ventricle and the blood cannot move forward. As the tricuspid valve does not close properly, all the blood from the right ventricle flows back into the right atrium (RA) in large quantities. This often results in significant dilatation of the right atrium.
How does a PA-IVS happen?
In fetal life, there is a defect in the development of the pulmonary valve. It is not known why this defect occurs. It is thought that there may be an inflammatory origin. Pulmonary valve obstruction can sometimes occur in twin gestations where there is a shared placenta for both twins and a disruption of the placental vessels.
Why is PA-IVS important?
PA-IVS can be associated with important anomalies in the heart and, less frequently, abnormalities in other body parts. In addition, it could be associated with chromosomal and genetic abnormalities. In type I there is a risk in pregnancy that the right ventricle will not develop properly, and in type II there is a risk of fetal heart failure and intrauterine death.
What are the things to watch for during pregnancy? Should I have more tests done?
- Prenatal diagnosis of a PA-IVS involves a detailed fetal ultrasound and an advanced echocardiography (a specialized ultrasound of the baby's heart during pregnancy) to rule out other associated heart defects or anomalies in other body parts.
- Parents should be offered an invasive technique to rule out associated chromosomal or genetic abnormalities.
- Monthly ultrasound monitoring is recommended to rule out signs of fetal complication as fetal heart failure (if valvular insufficiency is present). In addition, all cardiovascular structures should be evaluated at each scan.
- Intrauterine cardiac intervention in selected cases of PA-IVS may improve the prognosis of these fetuses.
Where should I deliver? Where will the baby receive the best care after it is born?
All patients with a prenatal diagnosis of PA-IVS should be born in a centre with high-risk pregnancy specialists, access to pediatric heart specialists, and an intensive care nursery.
What does it mean for my baby after it is born?
Once the child is born, the baby does not get enough oxygen in the blood. The main sign of oxygen deficiency is the presence of a bluish-purple discolouration of the skin and mucous membranes. Occasionally, there is also rapid and shallow breathing. After birth, it is necessary to treat the newborn immediately. Treatment of PA-IVS may include a combination of medications, procedures, or surgery to correct the congenital heart defect.
Will it happen again?
In the case of a previously affected child, the risk of recurrence is 1%; if two children are affected, the risk increases to 3%.
Last updated November 2022
