Supplement your learning for ISUOG's education course on early pregnancy complications.
Explore the topic before you attend our course:
In order to make the most of this learning experience and help you achieve your learning objectives, we have prepared a path to guide you from the essentials to our course’s topics through ISUOG resources. The material below will take you from the most basic aspects to a more comprehensive view of the course material, and some activities may grant you CME points.
Some of these activities are exclusively available to our members. Become a member today.
Spotlight on Ectopic Pregnancy by World Congress Faculty Member, Dr Nguyen T Ha
Ectopic pregnancy (EP) is characterized by the implantation and development of an embryo outside of the uterine cavity. The overall rate of EP is 1–2% in the general population, and 2–5% among patients who have utilized assisted reproductive technology. Although the overall mortality has decreased over time, ruptured EP is still the leading cause of maternal death during the first trimester with a mortality rate of up to 14%, and also responsible for approximately 5–10% of all pregnancy-related death. Prompt and accurate diagnosis is therefore of paramount importance to reduce pregnancy morbidity and mortality.
An ectopic pregnancy can be classified according to the location that the fertilized egg implants. Tubal EPs are the most common type, constitute over 90% of EPs, and non-tubal EPs comprise less than 10%. In some rare scenarios, the gestational sac can also be embedded in uncommon locations such as the cervix, ovary or abdomen. Furthermore, according to the classification of the European Society of Human Reproduction and Embryology (2020), extra uterine EPs (tubal, ovarian or abdominal EPs) refers to the gestational sac implanted outside of the uterus, while the embryo that is located within the uterus but breaches the endometrial–myometrial junction and extends into the myometrium should be described as uterine EPs (cervical, caesarean scar, intramural and interstitial EPs). Uterine ectopic pregnancies can be divided further into partial uterine EP if the location of the gestational sac inside the myometrium but partially protruding into the uterine cavity, and complete uterine EP if no visible communication between gestational sac and the uterine cavity can be seen.
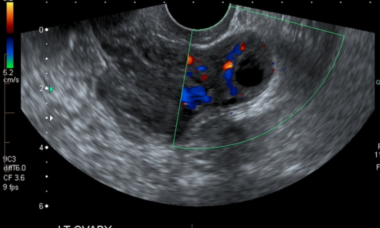
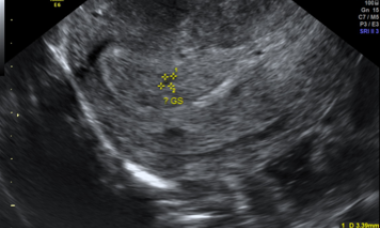
A comprehensive multidisciplinary approach should be obtained to establish an accurate diagnosis and management of EPs including a combination of accurate history and physical examination. Grayscale and color Doppler ultrasound (US) using both a transabdominal (TA) and a transvaginal (TV) approach are the first-line imaging modality when evaluating these patients. Transvaginal ultrasound is considered the primary diagnostic tool. Moreover, three-dimension ultrasound and MRI are important non-invasive methods in diagnosing partial uterine EPs because they are really useful to define the relationship between the gestational sac and endometrial–myometrial junction. These approaches would also help delineate the location of the gestational sac in equivocal cases. A single measurement of the quantitative β hCG level alone cannot provide sufficient evidence for the suspicion of an ectopic pregnancy. Therefore, serial quantitative β hCG levels correlated with serial transvaginal ultrasound findings are recommended to determine an early intrauterine pregnancy from ectopic pregnancy. A serial abnormal elevated beta β hCG levels can be helpful to suspect abnormal implantation but it should not be a useful marker to identify the locations of EPs.
Treatment strategies are vary depending on different factors such as the location of the pregnancy, hemodynamic status, the gestational age at diagnosis, serum β-HCG level, reproductive history and plan of future fertility. However, the most common interventions for the treatment of EP are medical management with systemic methotrexate and surgical removal of the pregnancy.
VISUOG
Ectopic Pregnancy
Explore the sub-sections on Uterine ectopic pregnancy, Extra-uterine ectopic pregnancy, and other rare sites.
Pregnancy of Unknown Location (PUL)
A PUL is defined as occuring when a patient tests positively for pregnancy but the initial transvaginal ultrasound scan is not able to locate the pregnancy. It is currently believed that the best way to manage these cases is by performing risk prediction, for which hCG and progesterone are used as biomarkers.
UOG Articles
Supplement your learning with specially chosen articles from UOG.
Reproductive outcome in 326 women with unicornuate uterus
T. Tellum, B. Bracco, L. V. De Braud, J. Knez, R. Ashton-Barnett, T. Amin, P. Chaggar, D. Jurkovic
13 September 2022
Ultrasound characteristics, serum biochemistry and outcome of ectopic pregnancies presenting during COVID-19 pandemic
C. Kyriacou, N. Cooper, E. Robinson, N. Parker, J. Barcroft, S. Kundu, P. Letchworth, S. Sur, D. Gould, C. Stalder, T. Bourne
04 October 2021
Recurrent Cesarean scar pregnancy: case series and literature review
I. E. Timor-Tritsch, G. Horwitz, F. D'Antonio, A. Monteagudo, E. Bornstein, J. Chervenak, L. Messina, M. Morlando, G. Cali
07 January 2021
Reproductive outcome after early miscarriage: comparing vaginal misoprostol treatment with expectant management in planned secondary analysis of randomized controlled trial
A. Fernlund, L. Jokubkiene, P. Sladkevicius, L. Valentin
15 September 2021
Predictive value of presence of amniotic sac without visible embryonic heartbeat in diagnosis of early embryonic demise
W. M. Dooley, L. De Braud, N. Thanatsis, M. Memtsa, E. Jauniaux, D. Jurkovic
04 November 2020
Learning modules
View lectures on similar subjects.
The evidence based management of pregnancy of unknown location (PUL) and the diagnosis of ectopic pregnancy
S Bobdiwala 2021
How can we accurately predict and diagnose miscarriage
J Preisler Romanow 2021
Avoiding diagnostic error when managing early pregnancy complications
T Bourne 2020
Embryo development by 3D
B Benoit 2018
CME activities
CME Activity: Do Events in Early Pregnancy Impact on Long-Term Pregnancy Outcome?
CME Activity: Tubal Ectopic Pregnancies: What Benchmark Detection Rate is Acceptable?
CME Activity: Caesarean Section Scar Pregnancy: Updates on Diagnosis and Management
CME Activity: Early First Trimester Detection of Fetal Malformation 8-11 Weeks
CME Activity: How to Manage Disorders Related to Implantation and Caesarean Section Scars in the Pregnant and Non-Pregnant Patient?